
The CARE Course

Critical Procedure - Tension pneumothorax
Back to Critical Procedures - Index page
For all procedures, ask yourself, 'does this need to be done 'now vs later'? And should this be done by 'me vs someone else?' Very often the answers will be 'now' and 'me' - so read on!
Tension pneumothorax
Description
 Emergency decompression of a tension pneumothorax using:
Emergency decompression of a tension pneumothorax using:
- intravenous catheter
- bespoke/dedicated catheter device
- open/finger thoracostomy
This procedure can be life saving but it can have complications so we need to select the right situation to perfrome it.
The presence of tension pneumothorax is not always an "all or nothing" thing - symptoms usually start fairly mildly and progress. That rate of progression can be rapid or considerably slower. The progression of symptoms might be our biggest clue.
Clear thought re pros and cons is important before we decompress a chest. How much do we suspect a tension? How sick is the patient? Can we perform an USS? Can we wait to try to be clearer about the diagnosis? .....all weighed against...if we think this is a tension and if we think it is markedly affecting the patient (extreme dyspnoea/tachypnoea, reduced ventilation (hyperexpanded, reduced breath sounds), hypotension, deteriorating in front of us) then we we need to act now.
In the absence of haemodynamic or significant respiratory compromise and without clear signs of a tension pneumothorax, we can pause, observe and attempt to clarify the diagnosis with USS, CXR or clinical findings...but watch for that progression.
Indications
Tension pneumothorax.
Traumatic cardiac arrest where tension pneumothorax is a possibility.
Contraindications
Significant doubt about the diagnosis and patient not in extremis.
Equipment
14 or 16G IV cannula - longer is better -
20ml syringe (not essential)
Skin prep
Optional - Heimlich valve or improvised Heimlich valve
Procedure
Needle decompression
Select site (ease, speed, chance of success)
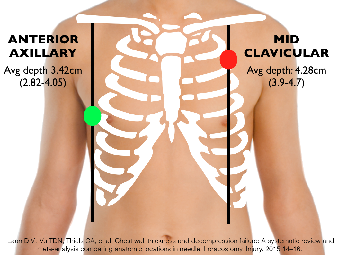
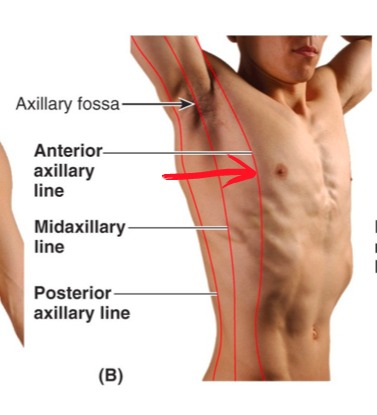
5th intercostal space in the anterior or mid axillary line (possibly higher chance of success than the traditional site, below)
OR
2nd intercostal space in the mid-clavicular line (the second rib joins the sternum at the Angle of Louis) - failure rate up to 50%
- brief skin preparation (if time allows), insert the cannula, perpendicular to the skin. Advance until you hear air escape.
- pull back the needle from the cannula, slide the cannula further in
- monitor for patency and re-occurrence
Finger thoracostomy
Open or 'finger' thoracostomy is a useful alternative that guarantees the chest cavity is decompressed and can provide diagnostic information.
NB Do not insert your finger if there is a rib fracture next to the insertion site - the bone will cut through your glove and into you.
- 4th or 5th intercostal space (ICS) in the anterior axillary line - i.e. the same location as will be used for the chest tube insertion which will need to follow it
- quick skin prep, lots of lidocaine local anaesthetic down to pleura
- incise the skin just above the 5th or 6th rib, about 1-1.5" in the line of the ribs (common error is to make this incision too small)
- put your finger in the hole
- use Kelly forceps to blunt dissect down alongside your finger to the pleura being careful not to push so hard as to overshoot into the chest when you pop through
- perform a finger sweep to confirm that you are into the chest and to obtain other information (can you feel the lung? is there blood? etc)
- if there is a rib fracture close then blunt dissect without your finger in, when you 'pop through' the pleura, hold the Kelly forceps in place, introduce the chest tube (loaded on a second set of Kelly forceps, along the forceps that are in place (this keeps your path into the chest cavity).
Potential pitfalls
Incorrect diagnosis.
Cannula too short and thus not reaching the pleural space.
Possible creation of a small pneumothorax from the cannula.
Haemorrhage.
Obstruction of the cannula by tissue leading to failed decompression.
Failure to follow up this procedure with formal chest tube insertion.
"Plan B"
If needle thoracostomy fails:
- attempt a second cannula and site
- open/finger thoracostomy ie. the first part of standard chest tube insertion - can be Plan A sometimes if can perform quickly
- chest tube insertion